Air ambulance providers in the United States could soon be required to distinguish between charges for air transportation and medical services in the bills they send to patients and insurers.

H.R. 4, the Federal Aviation Administration (FAA) Reauthorization Act recently passed by the U.S. House of Representatives, calls for federal rulemaking to require air ambulance operators to “clearly disclose charges for air transportation services separately from charges for non-air transportation services within any invoice or bill.”
Crucially, H.R. 4 also specifies that the “non-air transportation services” of air ambulance operators — and the prices thereof — are neither services nor prices of an air carrier for purposes of the Airline Deregulation Act (ADA). That could potentially open the door to state regulation of air ambulance billing — something that until now has been preempted by the ADA.
The Association of Air Medical Services (AAMS) and a related organization, Save Our Air Medical Resources (SOAR), are campaigning hard against the language in H.R. 4, warning that it would lead to “a patchwork of inconsistent state regulations” that could actually “put lives at risk” by impeding the transport of patients across state lines. SOAR represents some of the nation’s largest for-profit air medical operators, including Air Methods, PHI Air Medical, and Air Medical Group Holdings.
However, others in the industry have suggested that these fears are overblown. According to the Association of Critical Care Transport (ACCT) — which represents about 80 air and ground medical transport providers, many of them nonprofit or hospital-based — “there is nothing in the adopted House language which will change normal practice of serving critically ill and injured patients within and across state lines.”
With the Senate now considering its own version of the FAA Reauthorization Act, ACCT is urging Senators to retain the House language, arguing that it “effectively clarifies the appropriate role of state regulatory authorities in licensing and overseeing air medical programs . . . while protecting vulnerable patients in emergent events.”
A deregulated market
SOAR and ACCT have staked out their respective positions against a landscape of skyrocketing billed charges and rising consumer complaints. As the Government Accountability Office (GAO) noted last year, between 2007 and 2016, Air Methods increased its average price charged for an air ambulance transport from $13,000 to $49,800 — an increase of 283 percent. By contrast, during the same time period, the average price of medical care rose by about 13 percent and airline fares by just over 10 percent, according to the GAO.
Because air ambulance providers accept much lower reimbursement rates from Medicare and Medicaid patients — and may not receive any payment at all from uninsured patients — the impact of these rate hikes has fallen almost entirely on private healthcare insurers and their members. As billed charges have soared, more insurers have started limiting their reimbursements to air medical providers.
In some cases, providers who are not in network with insurers have gone after patients for the balance — leading to numerous news stories in which patients have described surprise bills for staggering amounts. For example, in one recent news story, Air Evac Lifeteam balance billed a Missouri family more than $32,000 for an 83-mile transport after the family’s insurer, Anthem Blue Cross Blue Shield, paid only $11,787 of a $44,232 bill.
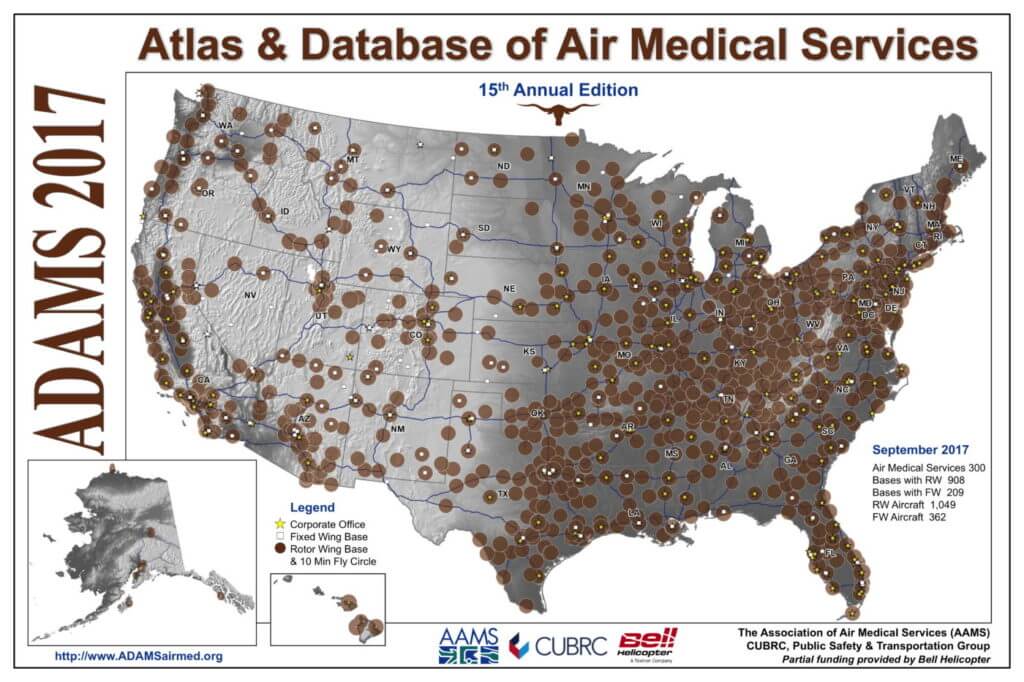
The rise in prices is related to an increase in the number of air medical helicopters. According to the Atlas & Database of Air Medical Services (ADAMS), there were 1,049 rotary-wing air ambulances in the U.S. in 2017, compared to just 545 in 2003. However, the number of patient transports has not increased proportionately, meaning that each air medical helicopter is now transporting fewer patients.
Most of the costs associated with running an air medical base are fixed — a provider must maintain an expensive aircraft and compensate highly trained pilots and clinicians no matter how many patients that aircraft transports. When those high fixed costs are spread across fewer transports, the average cost per transport rises, and providers must raise their prices to keep the same profit margin.
Air medical providers have given different explanations for why more helicopters are conducting fewer patient transports per aircraft. Some providers interviewed by the GAO said that the trend was due to helicopters increasingly being located in rural areas “where there is greater need, but less population density, leading to fewer transports per helicopter.”
However, the most recent ADAMS map shows that there are still many rural areas with limited air medical coverage, while other areas of the country have numerous bases with overlapping coverage areas. According to other providers interviewed by the GAO, the U.S. air medical industry is “oversaturated” and helicopters are being added in areas with existing coverage, “thereby reducing the average number of transports per helicopter rather than increasing access to patients previously not covered by the service.”
Air ambulance operators in the U.S. have been able to raise their prices to a much greater extent than the medical and airline industries generally due to the unique nature of the market, and the protections afforded to them as air carriers under the Airline Deregulation Act. Congress passed the ADA in 1978 with the expectation that competition between airlines would promote “efficiency, innovation, and low prices” for consumers. However, while airline passengers generally have the opportunity to comparison shop between airlines, few air medical patients have that luxury — many of them are transported under extreme duress, with little or no say in who flies them.
When patients and insurers do have the opportunity to comparison shop, free market forces appear to keep prices more closely aligned with costs. For example, in recent correspondence with the Department of Transportation, the consulting company Sentinel Air Medical Alliance cited numerous examples in which air medical providers charged insurers exorbitant amounts for patient transports, yet these providers or their competitors quoted brokers much lower amounts for the same transports arranged in advance.
In one instance, according to Sentinel, a provider charged $162,000 for a 259-mile transport in a 1982 Lear 35, yet three competing providers later quoted rates of between $6,750 and $9,000 for the same transport. “The discrepancy between what [the provider] charged the health plan for this service and what three other providers would have charged showcases the fact that markets work when present,” Sentinel wrote.
Yet courts have consistently struck down state attempts to control air ambulance prices and protect patients from balance billing. In 2015, North Dakota passed a law that established primary and secondary call lists for air ambulance service providers operating in the state. To qualify for the primary call list and receive priority in dispatching, air ambulance providers were required to sign in-network agreements with health insurance carriers representing at least 75 percent of the state’s privately insured population — which effectively required becoming a participating provider with Blue Cross Blue Shield.
Valley Med Flight challenged the law in U.S. District Court, contending that it would be unable to continue its operations in North Dakota if it was forced to accept rates mandated by Blue Cross Blue Shield, and that North Dakota’s law was preempted by a clause in the ADA that prohibits states from regulating the “price, route, or service of an air carrier.” In a March 2016 ruling, Judge Daniel L. Hovland sided with Valley Med Flight.
Hovland found that the purpose of North Dakota’s law was to prevent air ambulance providers “from imposing exorbitant fees on patients who wrongly assume their insurance will cover the charges,” and that “this type of consumer protection law is precisely the type of law Congress sought to preempt when it enacted the ADA.” He concluded, “No matter how noble the state’s intent in passing regulations or laws in this area, such acts are clearly preempted.”
Pushing for transparency
As it became increasingly clear that any effective consumer protection measures would need to start in Congress, air ambulance patients found an unlikely ally in U.S. Representative Rob Woodall, a Republican from Georgia’s 7th congressional district. Unlike many other states, Georgia hasn’t seen a rash of consumer complaints related to air ambulance billing. However, state insurance commissioner Ralph Hudgens had been following the issue, and suggested that Woodall get involved, according to Woodall’s spokesperson, Martin Wattenbarger.
“We were happy to lead on that,” Wattenbarger told Vertical. “We’re proud of the fact that our insurance commissioner was paying attention.”

Woodall’s office authored the language in H.R. 4 Section 412, “Advisory Committee for Transparency in Air Ambulance Industry,” which calls for the creation of a committee composed of representatives from government, health insurance providers, consumer groups, and various segments of the air ambulance industry. The committee would have 180 days to make recommendations on how to distinguish between air transportation and medical services on air ambulance bills. Then, the Secretary of Transportation would have a further 180 days to issue a final rule on the matter, and on other consumer protections for customers of air ambulance operators.
According to Wattenbarger, the language is “not about attacking an industry,” but rather ensuring that all actors in the air medical space are operating fairly. He added, “This is also about empowering our state insurance commissioners to be able to do the job they were elected to do — which is to protect consumers from predatory and unfair industry practices and ensure the free market in the healthcare industry works in Georgia, and other states, to promote more competition and better service.” On May 10, the Democratic Senator Claire McCaskill of Missouri introduced the language in the Senate in the form of S. 2812, the “Air Ambulance Consumer Protection Act.”
Opponents of H.R. Section 412 have focused their attention on paragraph (h), which states, “The non-air transportation services of air ambulance operators and prices thereof are neither services nor prices of an air carrier for purposes of section 41713 of title 49, United States Code” — the preemption clause of the ADA. By opening the door to more aggressive state regulation of these non-air transportation services, this language could “reduce access to air medical services and increase costs by causing states to regulate the industry differently,” said SOAR spokesperson Carter Johnson.
Johnson explained that most air ambulance providers operate in a regional capacity, with about 30 percent of all air medical transports taking place across state borders. If H.R. 4 Section 412 (h) were to lead to conflicting state regulations, she said, “this change would cause air medical providers to only look to in-state facilities, which could be farther away and less appropriate for the patient. In short, this seemingly small change could have a devastating effect on patients facing life-threatening emergencies, their access to care, and ultimately, their health outcomes.”
SOAR has argued that the onus for addressing patient balance billing should fall first on insurers, who “need to agree to a fair and reasonable reimbursement rate and drop demands for contract language that gives them power to overrule medical decisions by doctors and first responders who deploy air ambulances,” Johnson said. SOAR and AAMS are also advocating for legislation (H.R. 3378 / S. 2121) that would require providers to collect and submit cost data and bring Medicare reimbursements closer to the true cost of providing care, theoretically relieving pressure on privately insured patients to make up the difference.
“Because 70 percent of air medical patients have Medicare, Medicaid, or no insurance at all and Medicare reimbursement rates haven’t been updated in nearly 20 years, Congress must enact H.R. 3378 / S. 2121,” Johnson said.
A second opinion
However, others in the industry are skeptical of these arguments.
“Despite all of the noise there is no issue here,” said Tom Judge, executive director of LifeFlight of Maine and an ACCT board member. “H.R. 4 will not change any current practice but will help increase transparency of actual costs, which some fiercely resist.”

According to Judge, “the heart of the debate is whether states should be allowed to oversee ‘ambulance service’ — the provision of medical care whatever the actual vehicle. The ADA never anticipated an ambulance service would be conflated with an air carrier.”
As for whether a patchwork of conflicting state regulations will put patients’ lives at risk, Judge and ACCT executive director Roxanne Shanks find that unlikely. Shanks is the CEO of LifeFlight Eagle, a nonprofit air medical provider based in Kansas City, Missouri, that operates in both eastern Kansas and western Missouri. Shanks pointed out that states already regulate many aspects of the medical services that air ambulance operators provide, with little or no adverse effect on the patients under their care.
“We’re already licensed in both states that we fly in and out of, and we have to meet certain state requirements around the medical care and equipment that we provide,” she told Vertical. With respect to the language in H.R. 4 Section 412 (h), she said, “I don’t see, from my program’s perspective, that this would have any impact on what we do today as far as taking patients to the appropriate facilities and being able to cross state lines.”
Like AAMS and SOAR, ACCT supports legislation that would require air ambulance providers to submit cost data and raise Medicare reimbursement rates accordingly. However, while the bill supported by AAMS and SOAR provides for an immediate increase in reimbursement as that cost data is being collected, ACCT is supporting a different bill, H.R. 3780, that would only increase reimbursement after cost data has been analyzed.
“For ACCT, increasing reimbursement before they’re getting cost data just seems like putting the cart before the horse,” said Shanks. “It’s not that we don’t want to get paid more; absolutely, I’d like to break even on Medicare, that would be wonderful. But without any cost data . . . what are we asking for if we can’t truly show what our costs are?”
Shanks noted that previous increases in Medicare reimbursement rates incentivized growth in the industry, which exacerbated cost problems as competing providers placed “helicopters on top of helicopters.” Shanks said that LifeFlight Eagle has also seen its transport volumes drop with the proliferation of competing helicopters, and has had to raise its prices accordingly. However, the program has managed to preserve its positive relationship with private insurers, even as the battles between many for-profit operators and private insurers have intensified.
“We are fortunate that we’ve had a longstanding provider agreement with Blue Cross and Blue Shield of Kansas City and have for many, many years,” Shanks said. “We have a great relationship. We agreed on a reasonable rate, so we know the patient’s going to be covered [and] we’re going to be paid a reasonable amount, within a reasonable timeframe.”
Whether such an arrangement can once again become the norm in the U.S. air medical industry remains to be seen.










When they charge $30,000 for a 50 mile flight, something has to change.
The rates that HEMS is charging is absolutely outrageous. When the direct operating cost of the helicopter is roughly $1000-$1500 dollars per hour for an Astar 350 most flights are around 1.5-2 hours at the highest even say $4,000 how can you get from there to $50,000-75,000 dollars. That deal with the company in North Dakota, they wanted to use the helicopter rather than an airplane to transport patients due to the helicopter can charge more for the flight in most cases.
Having been in this industry for quite some time, the real issue starts with the dispatching and decision to fly a patient. A percent of patients are being transferred by air that do not need air transport, and would do just as well coming by ground ambulance. The issue starts with who is making the decision and their justification/motivation as well as the lack of defined criteria or why air vs ground is chosen. A fair amount of the time the decision to use air transport is subjective and not patient driven. Often little thought is given to the cost to the family by the decision makers, and more importantly if it is medically necessary and truly a “time sensitive” condition that warrants air transport.
Looking deeper into the problem of over use and abuse of this type of medical transport is where to start in terms of saving costs.